Regeneration is the reproduction or reconstruction of the lost or injured periodontal tissues in such a way that the architecture and function of the lost or injured tissues are completely restored. Procedures that regenerate lost bone and tissue supporting your teeth can reverse some of the damage caused by periodontal disease. Your periodontist may recommend a regenerative procedure when the bone supporting your teeth has been destroyed due to periodontal disease.
Regeneration
Regeneration
Ridge preservation is any procedure undertaken at the time of or following an extraction that is designed to minimize external resorption of the ridge and maximize bone formation within the socket.


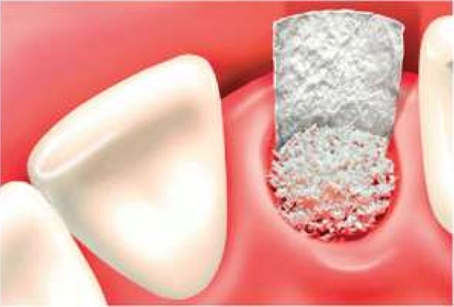
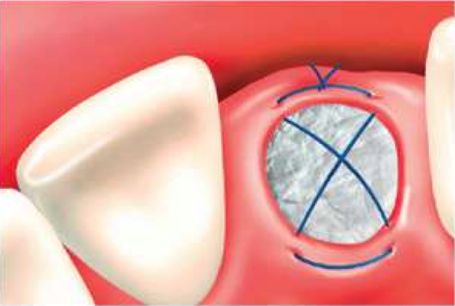
The resorption of bone following extraction may present a significant problem in implant and restorative dentistry. Ridge preservation is a technique whereby the amount of bone loss is limited. Following extraction of the tooth, bone grafting material is placed within the remaining socket and a resorbable membrane is placed between the bone and overlying soft tissue to allow the tissues mature over a 3-6-month post-operative period. Implant treatment can be facilitated at the time of extraction by considering ridge preservation and maintaining sufficient bone for optimal implant placement and consequently appearance.
Without Ridge Preservation

With Ridge Preservation

Gum disease has traditionally been treated by eliminating the gum pockets by trimming away the infected gum tissue and re-contouring the uneven bone. Although this is still an effective way of treating gum disease, new and more sophisticated procedures are routinely used today. One of these advancements is guided tissue regeneration (GTR). This procedure is used to stabilize endangered teeth that have deep bone defects around them.
As periodontal disease progresses, pockets of degenerated bone develops in the jaw. These pockets can promote the growth of bacteria and the spread of infection. To address these pockets, Dr. Shelby may recommend GTR. During this surgical procedure, the bone defect created by the bacteria is cleaned thoroughly, a bone graft is placed to fill the defect, a regenerative protein is added to enhance healing and a resorbable membrane is installed between the soft tissue and the pocket in the bone to “guide” healing. The membrane covers the bone defect so that fast-growing soft tissue is blocked and slower-growing bone can begin to grow and regenerate itself.
Surgical Procedure
The gum is opened with a procedure known as a flap. The area under the gums is cleaned out to remove all bacterial deposits and infection soft tissues. Then a membrane (with or without the bone graft material) is placed over the damaged bone.
Compartmentalizing tissues
Once in place over the bone and below the gums, the membrane provides necessary space and time for the bone to heal and start regenerating itself (defect fills in).
After healing
The stitches and membrane dissolve or are removed. In about 6 months, new attachments and bone regenerate to support the tooth or teeth.


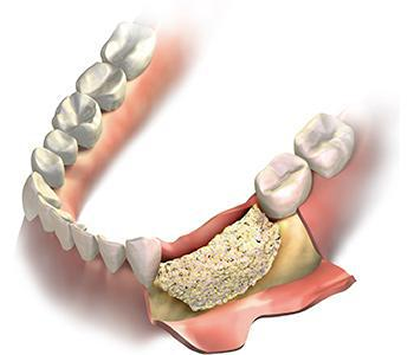 Over a period of time, the jawbone in the area of the missing teeth atrophies or is reabsorbed. This often leaves a condition in which there is poor quality and amount of bone to place an implant. In this type of situation, we now have the ability to grow bone when needed. This not only provides the opportunity to place an implant of proper length and width, it also enables us to restore functionality and an esthetic appearance. Bone grafting can repair implant sites with inadequate bone structure due to previous extractions, gum disease or injury. The bone is either obtained from a tissue bank or from the patient themselves. Bone grafting can also be placed in the sinus area to replace bone in the upper posterior areas and in large areas to repair defects. These defects can be the result of traumatic injury, tumor surgery or congenital defects. In severe cases, the ridge has resorbed, and a bone graft is placed to increase the height and/or width.
Over a period of time, the jawbone in the area of the missing teeth atrophies or is reabsorbed. This often leaves a condition in which there is poor quality and amount of bone to place an implant. In this type of situation, we now have the ability to grow bone when needed. This not only provides the opportunity to place an implant of proper length and width, it also enables us to restore functionality and an esthetic appearance. Bone grafting can repair implant sites with inadequate bone structure due to previous extractions, gum disease or injury. The bone is either obtained from a tissue bank or from the patient themselves. Bone grafting can also be placed in the sinus area to replace bone in the upper posterior areas and in large areas to repair defects. These defects can be the result of traumatic injury, tumor surgery or congenital defects. In severe cases, the ridge has resorbed, and a bone graft is placed to increase the height and/or width.

This technique is used to restore the lost bone dimension when the jaw is too thin to place an implant. The ridge of the jaw is expanded, the bone graft material is placed and allowed to mature for 6 to 9 months before placing the implant. This concept may also be utilized during implant placement to ensure adequate bone height and width to allow for proper placement with the intent of increasing long-term success.
Tooth loss in the upper jaw causes natural bone resorption and the sinking of the sinus cavity. The jawbone in this area is too thin and short to safely place a dental implant. A sinus lift raises the sinus cavity floor so bone graft material can be placed beneath, building up the necessary bone height and density for a dental implant post.
The upper back jaw (molar and premolar area) has traditionally been one of the most difficult areas to successfully place dental implants due to poorer quality of the bone that grows in this area as well as the close proximity of the maxillary sinus, an air-filled space within the upper (maxillary) jawbone.
When at least 5 mm of jawbone is present below the base of the sinus cavity, a sinus elevation via vertical approach can be performed. To perform this procedure, a set of drills that can cut the bone at the base of the sinus but not penetrate through the skin-like sinus membrane are used. Once the sinus membrane has been exposed, it can be further elevated with the introduction of a bone graft. Once sufficient bone height has been established, the implant can be placed during the same surgery. A crestal sinus elevation procedure can usually be performed when only a few millimeters of additional bone height need to be regenerated.
When there is minimal (less than 5 mm) bone present on the jaw below the base of the sinus, a sinus augmentation via lateral approach is needed. After 4-6 months, the implant can be placed if the proper amount of bone now exist.
